Americans should care about teen substance use because the developing brain is one of our nation’s most precious natural resources. We need our brains to create, innovate, and solve our country’s problems.
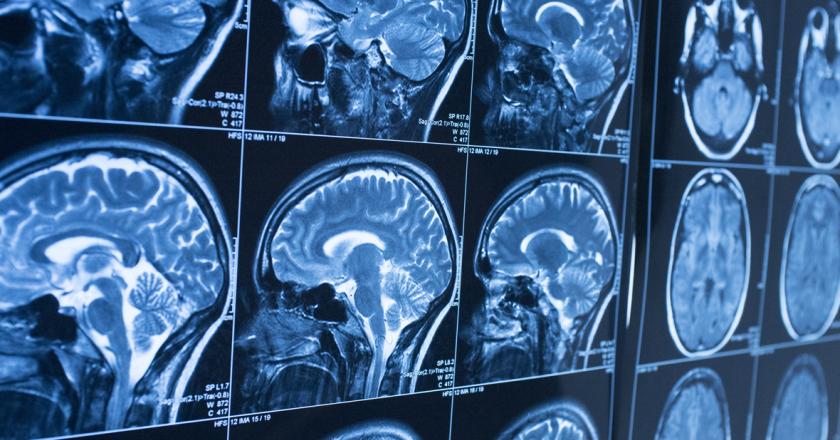
The brain goes through crucial changes in adolescence.1 Connections that are no longer needed are pruned. Fat cells, called myelin, develop around the neurons to provide insulation. The end result is to make the brain more efficient. Efficient brains, in turn, create our country’s future.
Unfortunately, adolescent substance exposure may interfere with brain development. 2 Brains that are exposed to alcohol, marijuana, opioids, and tobacco during adolescence are different from brains that are not exposed to these substances.3 They look different on brain scans, and they function differently as well. For these reasons, our country has an interest in preventing teen substance use and promoting healthy brain development.
In the area of teen substance use, we have cause for both celebration and concern. We celebrate decreases in the prevalence of teen drinking.4 At first glance, we might also celebrate decreases in teen cigarette smoking. However, if we include nicotine vaping, teens likely use more nicotine now than a decade ago.5 This increase is not surprising, given the way these products target youth with, among other things, sweet flavors such as chocolate, cherry, and vanilla.
Three main areas of concern are marijuana, opioids, and access to mental health/substance treatment.
- Marijuana. Among high school seniors, 6 percent use marijuana daily, and perceived harmfulness is at its lowest point ever with only 30 percent of high school seniors reporting great harm with regular use.6 Historically, perceived harmfulness is an important predictor of future use. Most striking is the legalization and commercialization of marijuana. Marijuana commercialization has led to cartoon advertising, brightly colored packaging, and sweetly flavored edibles (e.g., candy bars and sodas), all of which clearly target youth. Profits from selling these products can then be used to lobby and impede common-sense prevention such as plain packaging, limitations on potency, and restrictions on store hours.
- Opioids. Since 1999, the rate of people dying from opioid overdose has quadrupled.7 Adolescents have not been spared from the opioid overdose epidemic. From 1999–2013, drug overdose deaths among young people 12–25 years old increased from 3.1 to 7.3 deaths per 100,000.8 In 2015, 1.1 percent of all young people 12–17 years old, or 276,000 teens, used a prescription pain pill in the preceding month.9 Even when opioids do not lead to addiction or overdose, there is concern about their potential impact on the developing brain. For instance, animal models show that opioid exposure during adolescence promotes premature myelination of neurons.10 In other words, the precise sequencing of the brain development process is altered in potentially crucial ways.
- Access to substance treatment. Only 6 percent of adolescents with a substance problem access treatment.11 This treatment gap would never be tolerated for other conditions such as cancer, diabetes, and heart disease. Yet it has existed for years.
Our country’s future depends on healthy brain development. Adolescent exposure to substances endangers our future. In the 1970s, scientists discovered the ill effects of lead on the developing nervous system.12 Prevention efforts led to dramatic declines in the proportion of youth with toxic lead levels.13 Similar efforts are needed today to safeguard our youth—and our future—from drug and alcohol exposure.
Christian Thurstone, MD, is an Associate Professor at Denver Health and Hospital Authority/University of Colorado.
ENDNOTES:
1. Fact sheet, “The Teen Brain: 6 Things to Know,” U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health, NIH Publication No. OM 16-4307, https://www.nimh.nih.gov/health/publications/the-teen-brain-still-under-construction/index.shtml (accessed May 5, 2017).
2. Simon T. E. Baker, Murat Yucel, Alex Fornito, Nicholas B. Allen, and Dan I. Lubman, “A Systematic Review of Diffusion Weighted MRI Studies of White Matter Microstructure in Adolescent Substance Users,” Neuroscience & Biobehavioral Reviews, Vol. 37, No. 8 (September 2013), pp. 1713–1723, https://www.ncbi.nlm.nih.gov/pubmed/23845745 (accessed May 6, 2017).
3. Leslie L. Davidon, Elena L. Grigorenko, Michael J. Boivin, Elizabeth Rapa, and Alan Stein, “A Focus on Adolescence to Reduce Neurological, Mental Health and Substance-Use Disability,” Nature, Vol. 527, Issue 7578, Supplement (November 19, 2015), pp. S161–S166, https://www.nature.com/nature/journal/v527/n7578_supp_custom/full/nature16030.html (accessed May 6, 2017).
4. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health, September 2016, https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf (accessed May 6, 2017). Prepared for the SAMHSA by RTI International.
5. Jessica L. Barrington-Trimis, Robert Urman, Adam M. Leventhal, W. James Gauderman, Tess Boley Cruz, Tamika D. Gilreath, Steve Howland, Jennifer B. Unger, Kiros Berhane, Jonathan M. Samet, and Rob McConnell, “E-Cigarettes, Cigarettes, and the Prevalence of Adolescent Tobacco Use,” Pediatrics, Vol. 138, No. 2 (August 2016), http://pediatrics.aappublications.org/content/pediatrics/138/2/e20153983.full.pdf (accessed May 6, 2017).
6. Lloyd D. Johnston, Patrick M. O’Malley, Richard A. Miech, Jerald G. Bachman, and John E. Schulenberg, Monitoring the Future: National Survey Results on Drug Use 1975–2016: 2016 Overview of Key Findings on Adolescent Drug Use, University of Michigan, Institute for Social Research, January 2017, p. 82, Table 8, and p. 95, Table 11, http://monitoringthefuture.org//pubs/monographs/mtf-overview2016.pdf (accessed May 6, 2017).
7. U.S. Department of Health and Human Services, “The Opioid Epidemic: By the Numbers,” updated June 2016, https://www.hhs.gov/sites/default/files/Factsheet-opioids-061516.pdf (accessed May 6, 2017).
8. Li Hui Chen, Holly Hedegaard, and Margaret Warner, “Drug-poisoning Deaths Involving Opioid Analgesics: United States, 1999–2001,” U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, NCHS Data Brief No. 166 (September 2014), https://www.cdc.gov/nchs/data/databriefs/db166.pdf (accessed May 6, 2017).
9. Johnston, O’Malley, Miech, Bachman, and Schulenberg, Monitoring the Future: National Survey Results on Drug Use 1975–2016: 2016 Overview of Key Findings on Adolescent Drug Use, p. 82.
10. Allison A. Vestal-Laborde, Andrew C. Eschenroeder, John W. Bigbee, Susan E. Robinson, and Carmen Sato-Bigbee, “The Opioid System and Brain Development: Effects of Methadone on the Oligodendrocyte Lineage and the Early Stages of Myelination,” Developmental Neuroscience, Vol. 36 (2014), pp. 409–421, https://www.karger.com/Article/Pdf/365074 (accessed May 6, 2017).
11. Johnston, O’Malley, Miech, and Schulenberg, “Monitoring the Future: National Survey Results on Drug Use 1975 – 2016: 2016 Overview of Key Findings on Adolescent Drug Use,” p. 82.
12. President’s Task Force on Environmental Health Risks and Safety Risks to Children, Key Federal Programs to Reduce Childhood Lead Exposures and Eliminate Associated Health Impacts, November 2016, https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf (accessed May 5, 2017).
13. Ibid, p. 5.